 Are you ready "fore" golf?
Are you ready "fore" golf?
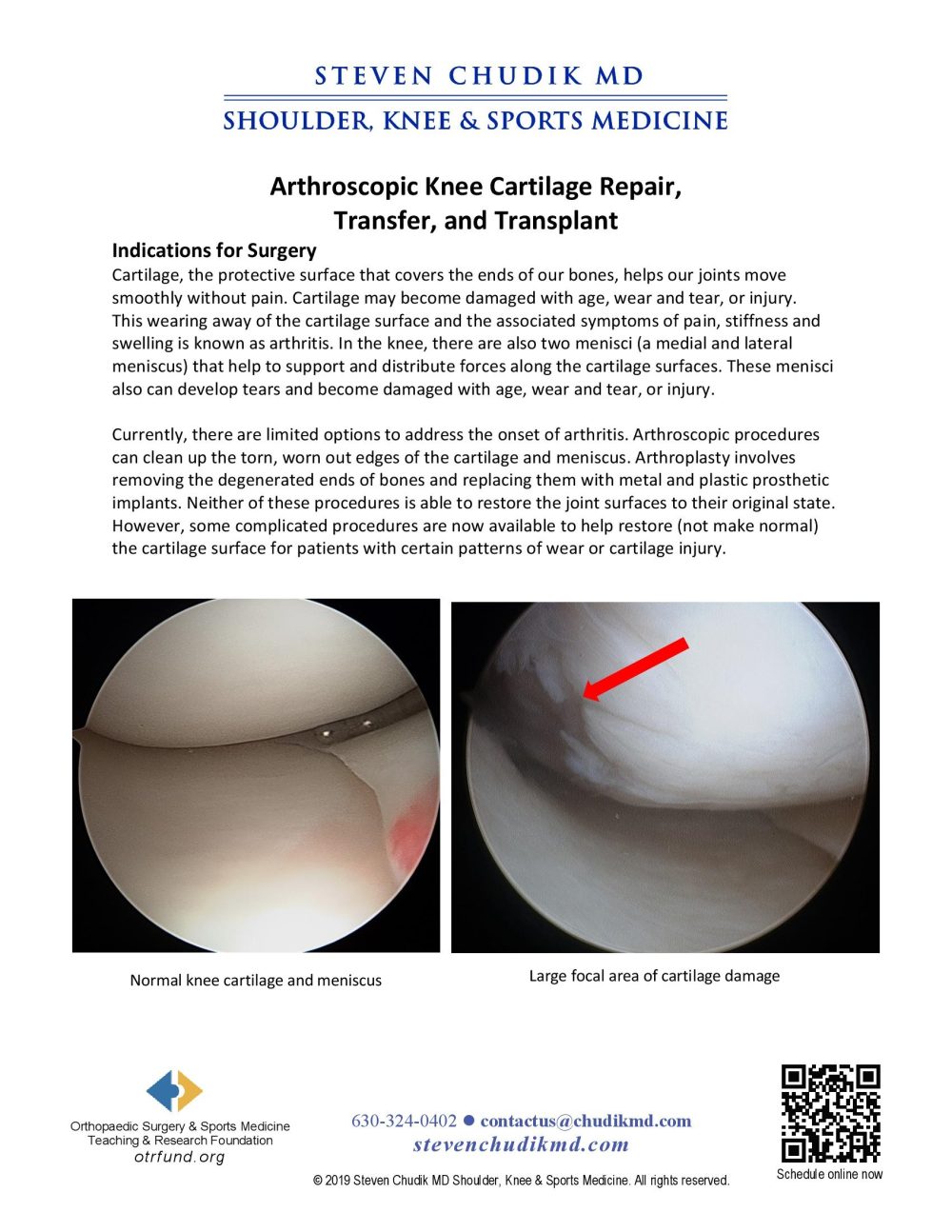
Cartilage, the protective surface that covers the ends of our bones, helps our joints move smoothly without pain. Cartilage may become damaged with age, wear and tear, or injury. This wearing away of the cartilage surface and the associated symptoms of pain, stiffness and swelling is known as arthritis. In the knee, there are also two menisci (a medial and lateral meniscus) that help to support and distribute forces along the cartilage surfaces. These menisci also can develop tears and become damaged with age, wear and tear, or injury.
Currently, there are limited options to address the onset of arthritis. Arthroscopic procedures can clean up the torn, worn out edges of the cartilage and meniscus. Arthroplasty involves removing the degenerated ends of bones and replacing them with metal and plastic prosthetic implants. Neither of these procedures is able to restore the joint surfaces to their original state. However, some complicated procedures are now available to help restore (not make normal) the cartilage surface for patients with certain patterns of wear or cartilage injury.
Learn More
Articular cartilage injuries do not heal and surgical repair still poses a difficult challenge. Following injury, the cartilage surface continues to wear, ultimately leading to arthritis and functional limitations. While significant advancements have been made in reparative procedures, all current methods are still unable to completely restore normal articular cartilage structure and function. As a result, we continue to search for better artificial materials and surgical techniques to restore the articular surface and allow long-lasting, painless joint function. The artificial surface materials tested were not able replicate the unique tribological properties of native cartilage. While normal cartilage produces negligible wear and has an inherently low coefficient of friction, the implanted materials resulted in higher coefficients of friction and increased cartilage wear. Polyurethane does, however, produce significantly lower friction and wear than chrome cobalt, which is commonly used for unipolar resurfacing of a joint. Further trials are planned to complete our study and determine if polyurethane is another potential material that can be used for repairing damaged cartilage surfaces.
Click here to learn moreArticular cartilage injuries are associated with joint trauma. Following injury, the articular cartilage surface continues to mechanically degenerate, causes accelerated degeneration of the opposing cartilage surface, and leads to functional limitations. Many of the current surgical approaches to treating isolated unipolar articular cartilage injuries fall short of restoring a normal articular cartilage surface. Therefore, we must confront the issue of altered tribological properties, continued degradation of the joint surface, and subsequent arthritis. The purpose of our study is to investigate the tribological behavior of bovine cartilage sliding against different artificial surface materials utilized in partial joint resurfacing. We hypothesize that through tribological studies, we will find the artificial material that least damages the opposing cartilage under dynamic loading force, and we will attain a better understanding of the mechanism of cartilage wear. We demonstrated that artificial joint resurfacing implants produce coefficients of friction that are higher than the coefficient of friction produced by the native cartilage in counter-surface reciprocation studies. However, all artificial materials do not produce equal coefficients of friction and the selection of material used in surgery should not be arbitrary. We showed that the coefficient of friction produced by the polyurethane counterface is significantly lower, and more equivalent to the coefficient of friction produced by the cartilage counterface, than the coefficients of friction produced by chrome cobalt and polyethylene counterfaces.
Click here to learn moreContent provided by Dr. Chudik not to be used for diagnosis and treatment. You can receive a proper evaluation and diagnosis by making an appointment with Dr. Chudik