 Because injuries are never planned, be prepared by bookmarking Dr. Steven Chudik's online scheduling tool today!
Because injuries are never planned, be prepared by bookmarking Dr. Steven Chudik's online scheduling tool today!
Anterior shoulder instability typically results from a dislocation injury to the shoulder joint when the humeral head (ball) of the humerus (upper arm bone) is displaced from its normal position in the center of the glenoid (socket) and the joint surfaces no longer touch each other. The most common dislocation is anterior (more than 90 percent), where the humeral head is in front and below the glenoid.
Because the shoulder has more motion than any other large joint in the body, it is the most commonly dislocated large joint. The shoulder is like a golf ball on a golf tee. Many structures contribute to shoulder stability and include bony contours of the humeral head (ball) and glenoid (socket), the soft-tissue bumper of the labrum which surrounds the rim of the socket, the capsule and ligaments that attach the humeral head to the labrum of the glenoid, and the muscles of the rotator cuff which surround the deep shoulder joint. When a shoulder is dislocated from its glenoid (socket), all these stabilizing structures may be injured to different degrees, including the humeral and glenoid bone, the labrum, the capsule and ligaments, and the rotator cuff muscles. When a younger active patient dislocates his or her shoulder, he or she may injure all these structures but typically tears the labrum off the glenoid (socket) along with the attached stabilizing capsule and ligaments, called a Bankart lesion.
Following reduction of a shoulder dislocation, functional outcomes are excellent and re-dislocation rates are low with proper treatment. For younger active patients, re-dislocation rates without surgical repair are extremely high and therefore, young athletic patients require arthroscopic repair of the injured stabilizing structures, most of the torn labrum, capsule and ligaments. For patients older than age 40, re-dislocation rates are lower, but the rate of rotator cuff injury is higher. Most patients over forty can be treated successfully without surgery unless a rotator cuff tear exists which requires operative repair in most cases.
Learn More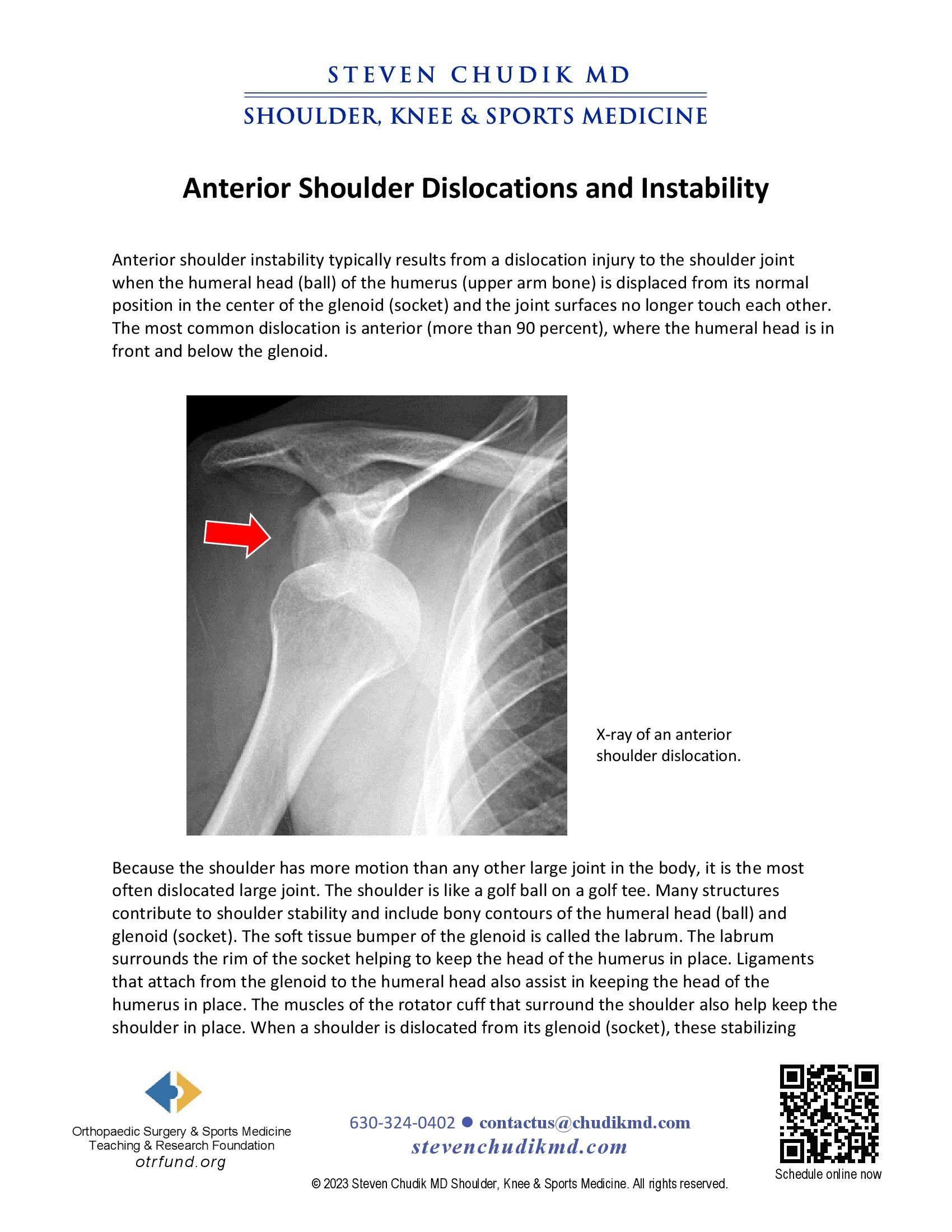
Content provided by Dr. Chudik not to be used for diagnosis and treatment. You can receive a proper evaluation and diagnosis by making an appointment with Dr. Chudik