Don’t drink caffeine for an energy boost---climb the stairs
Don’t drink caffeine for an energy boost---climb the stairs
Home / Arthroscopic Anatomic ACL Reconstruction
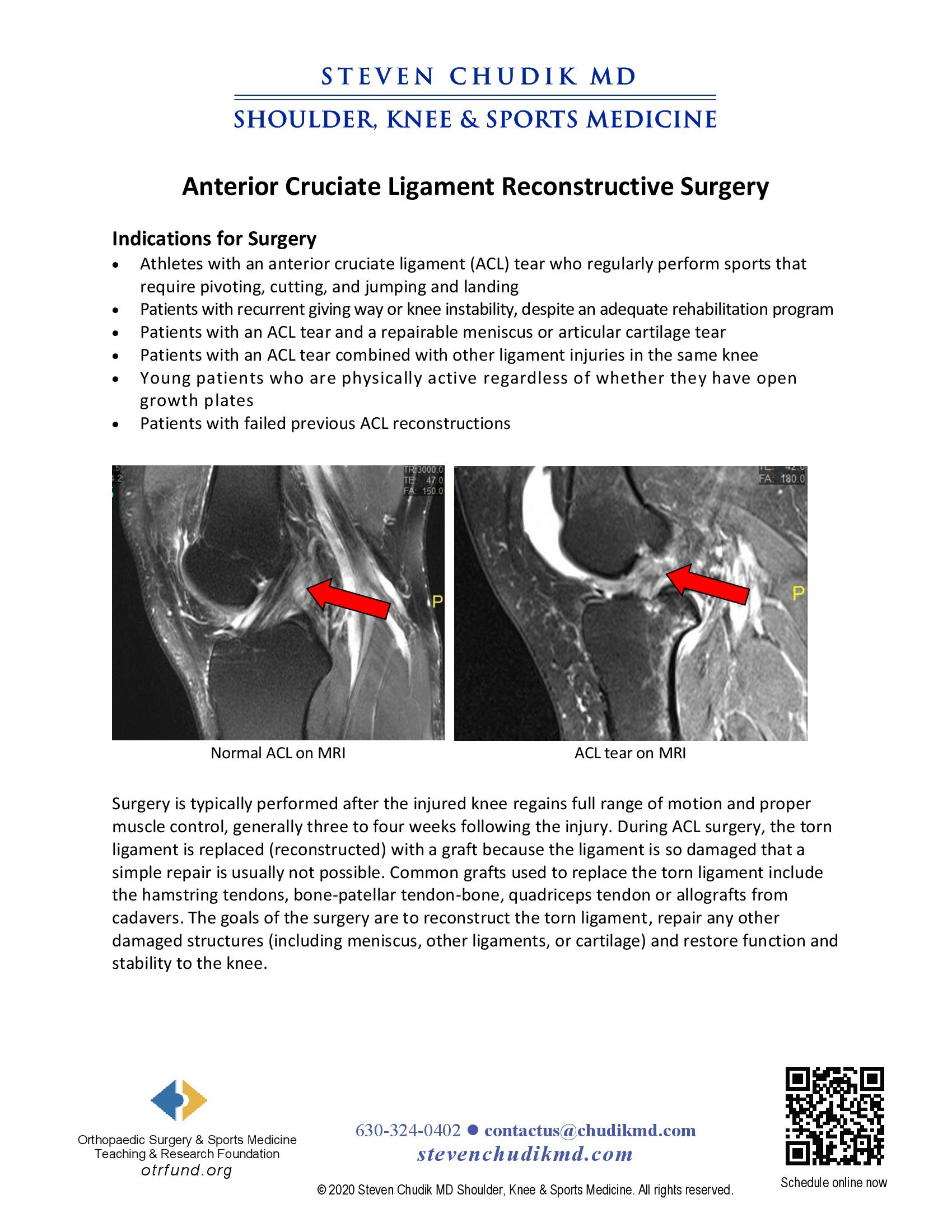
Surgery is typically performed after the injured knee regains full range of motion and proper
muscle control, generally 3 to 4 weeks following the injury. During ACL surgery, the torn
ligament is replaced (reconstructed) with a graft because the ligament is so damaged that a
simple repair is usually not sucessful. Common grafts used to replace the torn ligament include
the hamstring tendons, bone-patellar tendon-bone, quadriceps tendon or allografts from
cadavers. The goals of the surgery are to reconstruct the torn ligament, repair any other
damaged structures (including meniscus, other ligaments, or cartilage) and restore function and
stability to the knee.
click to learn more
Learn More
click to learn more
Learn More
 “Thanks Dr. Chudik for the great work getting my knee healthy so I can continue my football career at Lehigh next season. Go Mountain Hawks.”
“Thanks Dr. Chudik for the great work getting my knee healthy so I can continue my football career at Lehigh next season. Go Mountain Hawks.”
Dr Steven Chudik founded OTRF in 2007 to keep people active and healthy through unbiased education and research. Click to learn about OTRF’s free programs, educational opportunities and ways to participate with the nonprofit foundation.
1010 Executive Ct, Suite 250
Westmont, Illinois 60559
Phone: 630-324-0402
Fax: 630-920-2382
(New Patients)
550 W Ogden Ave
Hinsdale, IL 60521
Phone: 630-323-6116
Fax: 630-920-2382
4700 Gilbert Ave, Suite 51
Western Springs, Illinois 60558
Phone: 630-324-0402
Fax: 630-920-2382

© 2025 © 2019 Copyright Steven Chudik MD, All Rights Reserved.